ABSTRACT
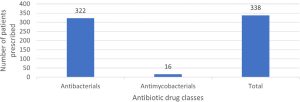
Background: Antibiotics are crucial for treating infections in older adults, but misuse can lead to drug-resistant bacteria, posing a global health challenge requiring urgent action. This study aimed to analyze the prescribing pattern of antibiotics among hospitalized older adults and identify factors influencing antibiotic use. Materials and Methods: This retrospective cross-sectional study focused on older adults hospitalized at Thumbay University Hospital, Ajman, UAE, for a period of 12 months. Patients with a hospital stay over 24 hr, receiving at least one antibiotic, were included. Data were collected using a standardized tool from electronic medical records and analyzed using classifications like Charlson Comorbidity Index and various WHO classifications, including AWaRe and INRUD prescribing indicators. Results: The study included 102 patients who received a total of 338 antibiotics. The most frequently prescribed class was systemic antibacterials, specifically cephalosporins and penems (41.25%). Piperacillin-tazobactam was the most used individual agent. High antibiotic prescribing rates related to skin and soft tissue infections (18.63%), pneumonia (18.04%), sepsis (17.75%), urinary tract infection (10.35%), and fracture and injury (8.57%). Patients generally received an average of 3.31 antibiotic agents. Most antibiotics prescribed were broad spectrum (81.95%), with 72.78% falling under the WHO AWaRe “Watch” group, indicating potential for resistance. Most antibiotics were from the national Essential Medicines List (82.24%) and prescribed using generic names (55.02%). The study also identified the total number of medications prescribed during hospital stay was found to correlate with the number of antibiotics prescribed. Conclusion: The study unveiled a divergence from the WHO antibiotic prescribing guidelines. It recommends conducting large-scale surveillance studies along with instituting institutional and national guidelines to curb antibiotic misuse and overuse in tertiary care hospitals.