ABSTRACT
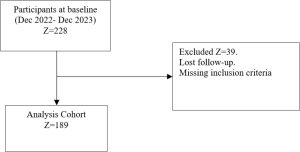
Background: Cardiovascular disease often advances rapidly in people with diabetes mellitus, resulting in unfavorable clinical outcomes and complications after revascularization procedures. The purpose of our study was to determine how baseline parameters and Diabetes Mellitus (DM) affected clinical outcomes in the immediate aftermath of revascularization. Materials and Methods: For this investigation, 189 patients who underwent CABG (Coronary Artery Bypass Graft) and PCI (Percutaneous Coronary Intervention) operations for revascularization during a five-month period in a South Indian tertiary care hospital were the subject of a hospital-based prospective observational analysis. During the first 30 days following revascularization, patients were assessed for clinical outcomes and baseline characteristics in the diabetic and non-diabetic groups. To ascertain the relevance of the findings, statistical analyses were carried out. Results: The study reveals that there is no statistically significant difference in the type of surgery, number of grafts or stents, urgency of the surgery, angiographic finding, length of ventilation, volume of the chest drain, stay in the cardiothoracic unit, and length of hospitalization between the diabetes and non-diabetic cohorts. Arrhythmia, stroke after revascularization, re-exploration within discharge mortality, pulmonary embolism, hemorrhage, perioperative mortality, and postoperative mortality within 30 days were evaluated as follow-up events in both the groups and determined to be insignificant. Conclusion: Even though prevalence of Cardiovascular Disease (CVD) is higher in diabetics, when comparing the diabetic and non-diabetic cohorts, it is not regarded as a risk factor for any negative outcomes following revascularization immediately within a period of thirty days following the angioplasty.